Aortic Health: Why One Size Doesn’t Fit All – The Rise of Personalized Medicine
For decades, managing ascending aortopathy (AA) – a weakening of the aorta, the body’s largest artery – has relied heavily on absolute size measurements. But groundbreaking research from the Cleveland Clinic’s Aorta Center, published in the Journal of the American Heart Association, is challenging this approach. The study reveals a stark reality: women with AA experience significantly poorer long-term survival than men, even when undergoing surgery at higher rates and presenting with fewer traditional cardiovascular risk factors. This isn’t simply a matter of statistics; it’s a call for a fundamental shift towards personalized aortic care.
The Gender Disparity: Beyond Diameter
Traditionally, a diameter of 5.5cm has been the benchmark for surgical intervention. However, the Cleveland Clinic study demonstrates that this threshold may be dangerously inadequate for women. A significant number of dissections and ruptures occurred in women *before* reaching this size. More than three-quarters of deaths and aortic catastrophes in women occurred when their aortic diameter was below 5cm. This highlights a critical gap in current guidelines.
The key lies in considering body size. Researchers found women exhibited significantly higher height-indexed measurements – Aortic Height Index (AHI) and Cross-Sectional Area to Height Index (CSAH) – than men, even with similar absolute aortic diameters. These indices account for individual body proportions, offering a more accurate assessment of risk. For example, a 5.2cm aorta in a shorter woman might be far more concerning than a 5.4cm aorta in a taller man.
Height-Indexed Metrics: A New Standard of Care?
The AHI and CSAH aren’t new concepts, but their widespread adoption has been slow. The Cleveland Clinic study provides compelling evidence for their integration into routine AA surveillance. The research suggests that intervention may be beneficial for women with an AHI below 3.21 cm/m, a threshold lower than previously considered.
This isn’t about lowering the bar for surgery; it’s about refining risk stratification. Consider the case of a 58-year-old woman, 5’4” tall, with a 4.8cm aorta and an AHI of 3.0 cm/m. Under current guidelines, she might be monitored. However, based on the new data, she may be a candidate for earlier intervention, potentially preventing a life-threatening dissection.
Beyond Sex: The Future of Aortic Risk Assessment
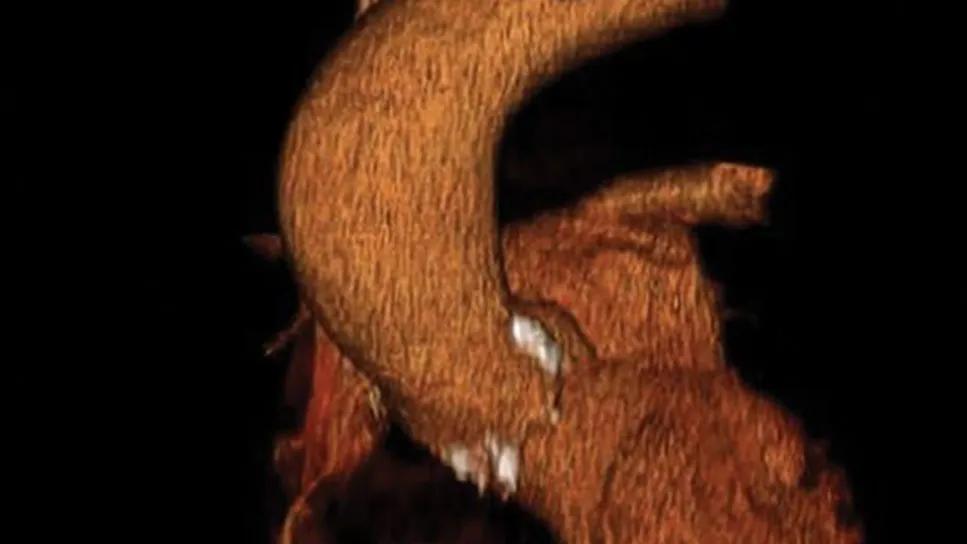
Personalized aortic care extends beyond gender. Researchers are exploring other factors that influence risk, including genetics, family history, and inflammatory markers. Advances in imaging technology, such as 4D flow MRI, are providing more detailed insights into aortic wall mechanics and blood flow patterns, allowing for even more precise risk assessment.
Artificial intelligence (AI) and machine learning are also poised to play a significant role. AI algorithms can analyze vast datasets of patient information to identify subtle patterns and predict which individuals are most likely to experience aortic events. This could lead to the development of personalized risk scores and tailored treatment plans.
The Role of Genetics and Biomarkers
Recent studies are uncovering genetic predispositions to aortic aneurysms and dissections. Variations in genes related to connective tissue, inflammation, and blood pressure regulation are being investigated. Furthermore, biomarkers – measurable substances in the blood – are being explored as potential indicators of aortic wall stress and vulnerability. For instance, elevated levels of certain matrix metalloproteinases (MMPs) have been linked to increased risk of dissection.
The Impact of Specialized Aortic Centers
The Cleveland Clinic study underscores the importance of seeking care at specialized aortic centers. These centers have the expertise, technology, and multidisciplinary teams necessary to provide comprehensive aortic care, including advanced imaging, genetic testing, and personalized surgical planning. Operative mortality rates are demonstrably lower at these centers, making them the optimal choice for patients with AA.
Frequently Asked Questions (FAQ)
Q: What is ascending aortopathy?
A: A weakening of the ascending aorta, the portion of the aorta that rises from the heart. It can lead to dissection, rupture, and death.
Q: What is AHI and CSAH?
A: AHI (Aortic Height Index) and CSAH (Cross-Sectional Area to Height Index) are height-indexed measurements that provide a more accurate assessment of aortic risk than absolute diameter alone.
Q: Should everyone with AA undergo genetic testing?
A: Not necessarily, but it may be recommended for individuals with a strong family history of aortic disease or early-onset aneurysms.
Q: How often should I be screened for AA if I have a family history?
A: Screening frequency depends on your individual risk factors. Discuss this with your cardiologist.
The future of aortic care is undeniably personalized. By embracing height-indexed metrics, incorporating genetic and biomarker data, and leveraging the expertise of specialized centers, we can move beyond a one-size-fits-all approach and provide more effective, life-saving care for all patients with ascending aortopathy.
Want to learn more? Explore additional resources on aortic health at the American Heart Association and Mayo Clinic.
Have questions about your aortic health? Share your thoughts in the comments below!