The Growing Crisis in Hospital Staffing: A Look at the Future
The recent protests by nurses at SSM Health St. Louis University Hospital highlight a nationwide trend: increasingly strained hospital staffing levels. What began as concerns over patient safety is rapidly evolving into a multifaceted crisis with implications for healthcare quality, worker well-being, and the future of hospital operations. This isn’t simply about needing more nurses; it’s a systemic issue demanding innovative solutions.
The Direct Link Between Staffing and Patient Outcomes
The core argument, as voiced by the National Nurses United/National Nurses Organizing Committee, is that inadequate staffing directly impacts patient safety. A recent study by the American Nurses Association found that hospitals with higher nurse-to-patient ratios consistently demonstrate lower rates of medication errors, hospital-acquired infections, and patient mortality. The SSM Health case, where a patient tragically died by suicide in the emergency department, underscores the potential consequences of overworked staff unable to provide adequate monitoring and emotional support.
Did you know? A 2022 report from the Bureau of Labor Statistics projects a shortage of 195,400 nurses each year through 2030, driven by an aging workforce and increasing demand for healthcare services.
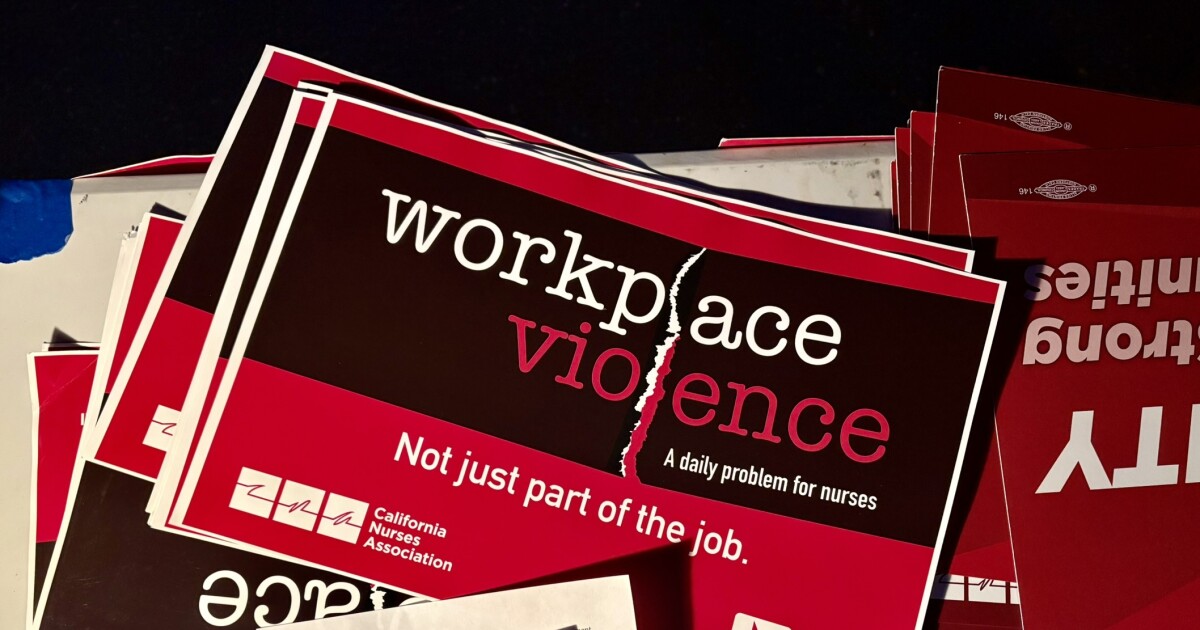
Beyond Nurse-to-Patient Ratios: The Expanding Scope of Hospital Security
The demands of nurses at SSM Health extend beyond simply increasing headcount. They are also advocating for improved security measures, particularly for charge nurses. This reflects a growing concern about workplace violence in healthcare settings. According to the Emergency Nurses Association, over 80% of emergency nurses have experienced verbal or physical assault on the job. This isn’t limited to emergency departments; all hospital units are seeing a rise in aggressive patient behavior, often fueled by mental health crises and substance abuse.
Hospitals are responding, as seen with the increased security presence at SSM Health following the November incident. However, security alone isn’t enough. The focus is shifting towards proactive de-escalation training for all staff, improved environmental design to minimize risk, and integrating mental health professionals into emergency care teams.
The Role of Technology in Addressing Staffing Shortages
While increasing staff remains a priority, hospitals are also exploring technological solutions to alleviate the burden on existing personnel. Telehealth is expanding beyond remote consultations to include remote patient monitoring and virtual rounding. Artificial intelligence (AI) is being used to automate administrative tasks, predict patient deterioration, and optimize bed management.
For example, several hospitals are piloting AI-powered systems that analyze patient data to identify those at high risk of falls or sepsis, allowing nurses to intervene proactively. Robotics are also playing a role, with robots assisting with tasks like medication delivery and linen transport, freeing up nurses to focus on direct patient care. Becker’s Hospital Review details several such implementations.
The Rise of Flexible Staffing Models and the “Gig Economy” of Nursing
Traditional employment models are being challenged by the rise of travel nursing and other flexible staffing arrangements. While these models can provide hospitals with temporary relief during staffing crises, they also come with drawbacks, including higher costs and potential disruptions to continuity of care.
We’re seeing a growth in platforms connecting hospitals with per diem nurses and other healthcare professionals, creating a “gig economy” within the healthcare sector. This trend raises questions about worker benefits, training standards, and the long-term impact on the quality of care.
The Impact of Burnout and the Need for Prioritizing Nurse Well-being
The chronic stress and exhaustion experienced by healthcare workers, particularly nurses, is a major driver of the staffing crisis. Burnout leads to increased turnover, reduced productivity, and a decline in patient care quality. Hospitals are beginning to recognize the importance of prioritizing nurse well-being through initiatives like mindfulness training, stress management programs, and improved work-life balance policies.
Pro Tip: Hospitals should invest in creating a supportive work environment that values nurses’ contributions and provides opportunities for professional development and growth.
Future Trends: Predictive Staffing and Data-Driven Resource Allocation
Looking ahead, the future of hospital staffing will likely be shaped by data analytics and predictive modeling. Hospitals will increasingly use data to forecast patient volumes, identify peak demand periods, and optimize staffing levels accordingly. This will require investing in sophisticated data infrastructure and training staff to interpret and utilize data effectively.
Furthermore, we can expect to see a greater emphasis on cross-training and skill diversification, allowing healthcare professionals to perform multiple roles and respond to changing patient needs. The integration of virtual care technologies will also continue to evolve, creating new opportunities to extend the reach of healthcare services and reduce the burden on hospital staff.
FAQ
Q: What is a safe nurse-to-patient ratio?
A: There is no universally agreed-upon ratio, but many experts recommend a ratio of 1:4 or 1:5 for general medical-surgical units, and 1:2 or 1:3 for intensive care units.
Q: How is technology helping with the nursing shortage?
A: AI, telehealth, and robotics are automating tasks, improving efficiency, and allowing nurses to focus on direct patient care.
Q: What can be done to address nurse burnout?
A: Hospitals need to prioritize nurse well-being through supportive work environments, stress management programs, and improved work-life balance policies.
Q: Will travel nurses continue to be a significant part of the healthcare workforce?
A: Likely, yes, but hospitals will need to find ways to balance the benefits of flexible staffing with the need for continuity of care and worker stability.
Want to learn more about the challenges facing healthcare workers? Explore the American Hospital Association’s insights. Share your thoughts on the future of hospital staffing in the comments below!